Study paper prepared by: Suhasini Bali and MihikaBapna
ABSTRACT
Over the time, the Government of India has launched multiple programs and policies to achieve the targets under millennium development goals. While the country showed improvements in health indicators, the progress has been sub optimal. With low share of institutional deliveries, India still accounts for high IMR, MMR rates with rising healthcare cost and out of pocket expenditure. Day by day the gap between urban and rural healthcare is also increasing, making healthcare debilitating for rural areas. Jharkhand is the 28th state of India with 76% rural inhabitants out of which 28% are Scheduled Tribes. It also has low female literacy (56%) with a large number of girls marrying before the legal age 18yrs.
The widespread poverty, malnutrition, coverage of health-care services, being far below the IPHS norms, absence of safe drinking water, food insecurity and sanitary conditions are some other factors of dismal health in Jharkhand.
Despite the tremendous strides made in reducing the deaths of women and children through policies and programs, health is still an area of concern in the state. Hence, this paper is an attempt to explore the current status of the healthcare services in Jharkhand, assesses gaps and explores recommendations to achieve the aspiration of health for all. Deliberation of the current healthcare status will enable the stakeholders to understand the existing structural approach of the policies and identify areas that need attention.
INTRODUCTION
Public Health is defined as “the art and science of preventing disease, prolonging life and promoting health through the organized efforts of society” (Acheson, 1988; WHO). Public health system across nations is a conglomeration of all organized activities that prevent disease, prolong life and promote health and efficiency of its people. Indian healthcare system has been historically dominated by curative practices focussing more on provisioning of medical care whereas the preventive and promotive aspects have been less emphasised.
The public health care system was originally developed in order to provide a means to healthcare access regardless of socioeconomic status or caste. Decisions on different factors related to public healthcare are taken majorly by the national government. The national government addresses broadly issues such as overall family welfare and prevention of major diseases, while the state governments handle aspects such as local hospitals, public health, promotion and sanitation, which differ from state to state based on the particular communities involved.
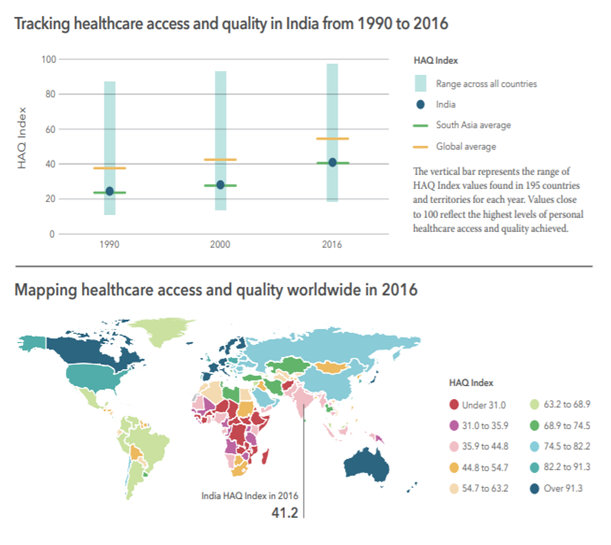
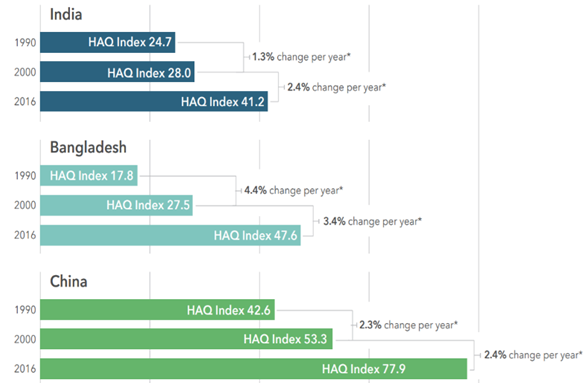
- The regional differences in India and China could be due to multiple reasons such as large variations in physical access to health facilities, the state of health infrastructure, the level and scale-up of medical technologies, and the provision of effective services across the spectrum of care, the study said.
- The healthcare system of India is lacking in three factors related to access to healthcare: provision, utilization, and attainment. Provision, or the supply of healthcare facilities, can lead to utilization, and finally attainment of good health. However, there currently exists a huge gap between these factors, leading to a disrupted system with issues of access to healthcare. Differential distributions of services, power, and resources have resulted in inequalities in healthcare access (Balaranjan, 2011).
- Access and entry into hospitals depends on gender, socioeconomic status, education, paying capacities, and location of residence (urban versus rural) Furthermore, inequalities in financing healthcare and distance from healthcare facilities are barriers to access.
- There is an urgent need to establish systems as per the IPHS norms as there is lack of sufficient infrastructure in areas with high concentrations of poor individuals otherwise health systems could face widening gaps between the health services they provide and the disease burden in their population.
Generally, countries that spent more on health per capita and had better health systems scored higher on the HAQ index, the study found. This strengthens the case for India to increase its healthcare spending. India spends just 1.4 percent of gross domestic product (GDP) on health, as IndiaSpend reported on 30 January 2018, creating a healthcare crisis that is holding back the country's potential. The World Health Organisation recommends that countries spend 4-5% of their GDP on health to achieve universal healthcare.
The healthcare allocation in the Union Budget 2020-21 is just a modest increase of 5.7 per cent to Rs 67,484 crore from the revised estimate of Rs 63,830 crore in the previous year and falls short of the target of spending 2.5% of GDP on healthcare. The public sector spend on healthcare will continue to lag, at below 1.5% of GDP.
India spent barely 1.29% of its gross domestic product (GDP) on healthcare in the financial year 2020, an April 7 report from CARE Ratings says. The spending on capital expenditure was worse, at only 0.19% during the period of pandemic COVID-19 as per the article posted in Business Today around union budget spending. Such prolonged scenarios of pandemic assume resources and medical staff to be reassigned to covid-19 patients. They also include delays in regular antenatal and postnatal care due to the fear of getting infected at the health facility, and medicine and vaccine shortages.
Jharkhand is one of the empowered states which still continue to share a number of characteristics with other backward states of India such as high infant mortality, low immunization of children and expectant mothers, high mortality due to infectious and contagious diseases, high maternal mortality and low institutional delivery. These added with poor accessibility to health care facilities and high cost of treatment by households have made all the achievements in the health sector insignificant. Despite the National Health Mission (NHM) and Government’s commitment to improve the availability of and access to quality health care by people, especially for those residing in the rural area, though progress has been recorded but still there is scope for significant improvement to be seen in the public health indicators in the state.
Many factors contribute to the poor health status including poverty, poor infrastructure and high morbidity. Poverty associated communicable diseases like tuberculosis and malaria along with maternal mortality and morbidity comprise a major portion of the disease burden. The health care status can be best understood by assessing the status of the indicators relating to it. Health indicators describe the health care needs of a population and reflect the functioning of health care interventions. In this paper we will be studying few of the indicators to produce more light on the status of healthcare of Jharkhand.
- Infant Mortality Rate (IMR): Infant Mortality Rate (IMR) is the number of infant deaths (less than one year) per thousand live births. Premature birth has been the biggest contributor to IMR, in addition to Pneumonia, birth asphyxia, birth complications and malnourishment. Disease like malaria, diarrhoea and measles.
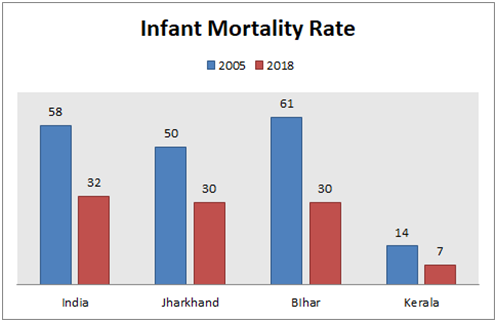
❖Multiple factors for status in IMR in Jharkhand:
- Institutional deliveries and distribution of IFA tablets to pregnant mothers have strengthened which have helped reduce the IMR.
- Premature birth rate has been one of the contributing factors for rise in IMR.
- Other contributing factors are pneumonia, birth asphyxia, malnourishment, birth complications, diseases like malaria, diarrhea, and measles.
- Special focus needs to be given in antenatal and neonatal care through immunization and other programs to continue improving IMR.
- Maternal Mortality Rate (MMR): It is defined as the number of maternal deaths during a given time period per 100,000 live births during the same period. Medical and socioeconomic factors majorly lead to maternal mortality and are largely preventable.
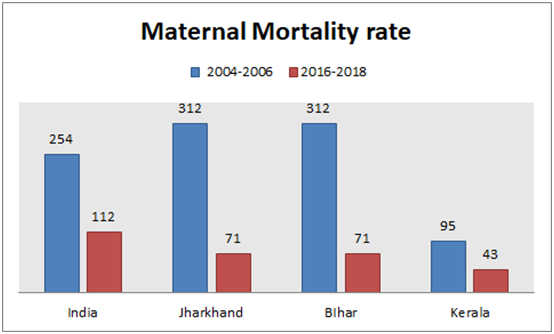
❖ Multiple factors for reduction in MMR in jharkhand:
- There was an increased emphasis as well as number of institutional deliveries.
- In 2014-2015, the ambulance service was introduced for expecting mothers to be carried to hospitals.
- More health sub-centres were equipped for handling deliveries, this increased the number of delivery points in the state.
Janani Suraksha Yojana(JSY) which was introduced since NRHM was launched guaranteed monetary help and encouraged women to choose institutional deliveries. in 2011, Janani Shishu Suraksha Karyakaram (JSSK) to eliminate out-of-pocket expenses for both pregnant women and sick infants. It ensured transportation of pregnant women from home to institution, free surgery including blood transfusion , medicines upto 42 days of delivery to mothers and medicines up to 1 year for the child.
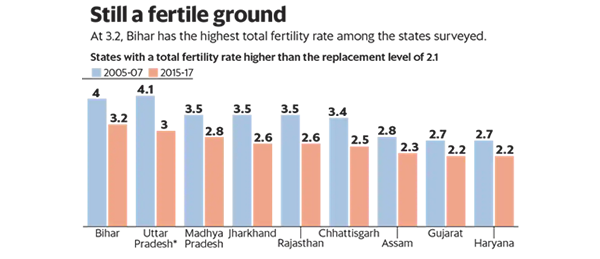
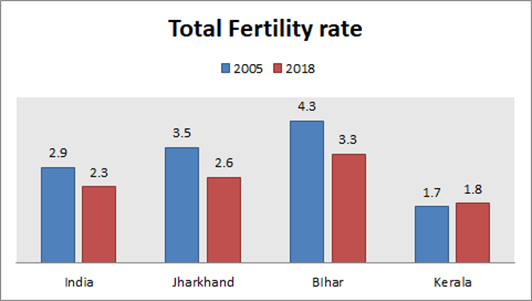
- Total fertility Rate (TFR): TFR is the most commonly used measure of fertility. It represents the number of children that would be born to a woman if she experiences the current fertility rate throughout her reproductive age of 15 to 49 years. In developing countries, high level of fertility is linked to poverty, female literacy, gender inequality, low female labour participation rates, and other measures of social and economic development
- In India, the total fertility rate has declined from 3.6 to 2.3 during 1991 to 2016. In 2016, around 80.8 percent of the deliveries were institutional which includes Government as well as private hospitals. The percentage of institutional deliveries in urban areas is 94.2 as against about 76.1 percent recorded in rural areas.
❖ Possible reasons for rise and fall in TFR:
Higher education, increased mobility, late marriage, financially independent women and overall prosperity are all contributing to a falling TFR. It goes below 2 in both urban and rural areas, where girls complete schooling and reduces further as they pass college. Bihar, with the highest TFR of 3.2, had the maximum percentage of illiterate women at 26.8%, while Kerala, where the literacy rate among women is 99.3%, had among the lowest fertility rates. As more cities come up, people move for jobs and employment tenure gets shorter, TFR may fall further.
Jharkhand has rampant poverty, poor health infrastructure and accessibility to health care services. Lack of safe drinking water, poor sanitation, hygienic condition and nutritional status are emerging concerns which make the women and children more vulnerable to ill health. Cultural norms and values, gendered division of work at home, gender discrimination, violence further push women to strive more for good health.
Nutritional status of women directly impacts their reproductive and sexual health and their child’s health status. Anaemia is a major concern among women all over India and more so in this belt with high rates of IMR and MMR. Keeping these issues as central Jharkhand is one of the high focused states under the National Rural Health Mission. This section gives a brief about some of them.
1. NATIONAL HEALTH MISSION
Ever since independence, various Health schemes and programs have been launched to improve the health status of people living in rural areas. The Government launched the National Rural Health Mission (which is now called National Health Mission) in 2005 throughout the country which aimed to provide universal access to equitable, quality and affordable health care. It focuses on providing Maternal, Children and Adolescent Health services as well as strengthening the community process to deliver health services up to village level along with an enhanced budget and scope for innovation in the health sector. This has helped in reducing the burden of communicable diseases and helped the nation to take huge strides in reducing maternal and child mortality and combating communicable diseases such as malaria and tuberculosis etc.
Women’s and Children’s health programs are at the very core of NHM. Some of its schemes are:
This initiative was started to ensure better and free facilities for maternal to pregnant women to encourage institutional deliveries. Under this, a pregnant woman is entitled to free and cashless delivery, free transport to the health facilities, free diet and drugs during the stay at the health facility, free provision of blood and exemption from user charges. For implementation of all the above schemes, NHM introduced the concept of ASHA (accredited social health activist) known as Sahiya in Jharkhand as a central agent in the community health programs. The role of Sahiya is to bridge the gap between the healthcare system and community. With their functioning, there has been an increase in village level awareness around maternal health and safe delivery practices
- This promoted safe delivery practices in Jharkhand though concerns like incentive disbursement, quality of service delivery and program management were being raised from several sectors. Jharkhand has 42000 Sahiyas . As per NHFS 4 data, 61.9% institutional deliveries were reported which is a low number hence the program needs to further strengthen.
12 - MUKHYA MANTRI JANANI SHISHU SWASTHYA ABHIYAN: The JSY program under NHM as described above is named as MukhyaMantri Janani Shishu Swasthya Abhiyan (MMJSSA) in Jharkhand in 2006 under which Rs 1400 is given as cash assistance to all pregnant women who deliver in public health facilities.
Jharkhand, being a difficult geographical terrain, promoted availability of transport but still many women deliver at home due to inaccessibility of facility or transport and other sociocultural factors.
To reduce the delay in referral during childbirth and the treatment of sick newborn, free referral services to the health facilities for the beneficiaries is achieved through availability of vehicles referred to as Mamta-Vahans.
- The MCP Card is a maternal and child care entitlement card, a counselling and family empowerment tool which ensures tracking of mother and child for health, nutrition and development purposes. It has the potential to create awareness, facilitate community dialogue and generate demand for uptake of vital services being provided. The card is for pregnant, lactating women and families with children under 3. It has the details of all government schemes, record of pregnancy and regular check-ups, antenatal care check-ups, postnatal care and child care services and visits. For children, it includes common diseases, developmental milestones and feeding practices for awareness of mothers.
- PRADHAN MANTRI MATRU VANDANA YOJANA
As mentioned above, poor nutrition status of women and children, prevalence of anaemia and malnutrition adversely affect women’s health. Poor health and nutrition during pregnancy can lead to poor health of children and it extends to their lifetime. Thus, this scheme was introduced using the platform of Anganwadi where an incentive of 5000/- is provided to pregnant or lactating women for their first child to improve their health seeking behaviour and compensate any wage losses. Given a long institutional delivery benefit (JSY) an average of 6000/- is given to the woman. As per an RTI filed by some activists about PMMVY coverage, Jharkhand reported 21.9% coverage of all births who have received at least one instalment. 22
- AYUSHMAN BHARAT PROGRAMME
To reiterate strengthening of primary health care, The National Health Policy (NHP) 2017 launched another ambitious Ayushman Bharat Programme in 2018 to deliver Preventive, Promotive and Comprehensive Primary Health Care through two major health initiatives, namely Health and wellness Centres and National Health Protection Scheme. It envisages not just providing a healthcare delivery system but through these Health and wellness centres, population-based screening for non-communicable diseases has been one of the priority initiatives taken by the state of Jharkhand under this program and this has helped in early identification, prompt treatment and regular follow up of NCD cases. It also introduced Pradhan Mantri Jan ArogyaYojana (PMJAY), a health insurance cover to more than 107.4 million poor and vulnerable families. In Jharkhand, over 46,000 odd claims have been raised so far; of which 80 per cent are from private hospitals raising the concern of if it is reaching the most marginalized. 24- The scheme promises customers what they have always expected, free quality treatment for up to Rs 5 lakh, however, poor people at hospitals expecting cashless treatment are paying a considerable amount. In Jharkhand, they are struggling to understand why their treatment can’t be free when the government has promised up to Rs 5 lakh. 25
- INTEGRATED CHILD DEVELOPMENT SCHEME (ICDS)
The Scheme provides an integrated approach for psychological development of the children of 0-6 age group, improves their nutritional & health status and reduces incidence of mortality, morbidity, malnutrition through community-based workers and helpers. It focuses on Nutrition and Health Education, supplementary nutrition, Immunization, Health Check-up and Referral services. The scheme has addressed hunger and but still there are numbers of children with malnutrition in Jharkhand putting a question mark on the efficacy of the schemes. In Jharkhand, a large number of children are living under poverty line, anaemia and malnutrition is prevalent and the share of children aged 0-6 years in the population (17.8 per cent) is higher than the national average (15.4 per cent) resulting the need for effective implementation of this programme.26
- CORONA AND HEALTH STATUS OF WOMEN
In 2019, the nation was hit by Noval corona virus, now popularly known as COVID-19. The pandemic is deepening pre-existing inequalities in India amplifying the impacts of the pandemic. Right to health of people and its implicit connections with their overall lives have been highlighted in this time of pandemic. Further in Jharkhand, healthcare remains within the discourse of the existing poor health infrastructure, availability and accessibility and women are facing additional burden of their access to Health and are vulnerable to Gender-based violence - The health of survivors of gender-based violence is further marginalised during this period. Freedom from violence is a significant determinant of women’s health. There is a need for a public health response to this concerned cause.
- A study shows that nearly 1.85 million women’s access to MTP services was severely affected in Pandemic which is a clear violation of their health rights. (IPAS Development Foundation, 2020)
- Sexual and Reproductive health services are also affected: Daily media reports and community engagements seem to reinforce the realities of the unfolding crisis faced by many women like migrant women are being forced to deliver on roads. Decreasing numbers of institutional deliveries and ANC checkups during this time may adversely affect the improved health indicators.
- In India, on an average, a government doctor attends to 11,082 people, more than 10 times than what the WHO recommends. In Jharkhand, the number is 18,518. Thus, COVID 19 response & reallocation of health services should not undermine the access to essential sexual and reproductive health services.
- The dismal working conditions of frontline workers such as Sahiyyas must be improved. There is a need to address their demand and build local support for them and other frontline workers so they are motivated to keep performing their role as maternal and child health educator.
- There has been a reduced frequency of meals of women along with loss of livelihood, and the worst hit group is the tribal women which comprises a large population in our state.
Hence, this calls for a collaborative response that does not deepen existing inequalities and violate women’s dignity, autonomy and voice.
- CORONA AND HEALTH STATUS OF WOMEN
- In above sections, it is explicit that the state has alarming IMR and considerable MMR rates whacking from undernutrition, anemia and other socio-economic factors. According to NHFS 4, out of all children below 5 years, 56.5% are underweight, 45.3% are stunted and 29% are wasted. Though there has been a slight improvement reported if we compare it to NHFS 3 data but it is evident that there is a need to strengthen the ongoing programs and explore the constraints and areas that need to be focussed.
-
Women in the state have a higher probability of bearing multiple burdens of social exclusion, poverty and being a woman in patriarchal society. Many studies around maternal and child health have reported poor nutritional status of women resulting in high morbidity and mortality. This is coming from low utilization of antenatal and postnatal services, unavailability of services, anaemia and malnutrition among tribal women in the state. As per NHFS4, Percentage of mothers who have 4 antenatal visits is 30.3%, mothers who had antenatal check-up in the first trimester is 52% and total Institutional Births is 61.9%. 31
A Study based on Jharkhand’s health shows that poor infrastructure, lack of quality care, behaviour of the health personnel, lack of information, difficult terrain, poor transport are the major factors for poor utilization of maternal health care. The health and nutritional status of the community is also associated with their housing and sanitation condition, livelihood status, dietary intake, socio culture beliefs and accessibility to healthcare. Infant mortality is closely associated with maternal and child health care practices. Though there is an increase in institutional deliveries, many women are still delivering at home due to inaccessibility and other cultural factors that affect their health seeking behaviour. Not having decision making choices for their own health, women silently bear reproductive health problems and ignore it.
Through NHM, health system effectiveness has expanded along with rising institutional deliveries which have brought down the maternal mortality ratio (MMR). However, India still accounts for 19% of global maternal deaths and Jharkhand’s share is considerable in that making it far from achieving the fifth MDG target. Women with complications avoid seeking care in a facility if they had a previous experience of disrespectful treatment at a health care facility.
Of all the above described schemes and policies, Primary health care (PHC) has been the central of them all which is facing a major healthcare challenge in India. There is a lack of robust infrastructure and human resources. There is a 60% shortfall of PHCs, 22% shortfall in the required number of sub centres and among them only 44% of the sub centres are functioning in a government building, and merely 15% of them have an ANM. Existing PHCs even don’t have regular supplies of electricity and clean water. Secondary and tertiary health care are also lacking skilled workforce and there is a growing concern around its quality. Concerted efforts are required to strengthen the services and link it to higher levels of care.
There is a gap in infrastructure, quality care and accessibility to strengthen public healthcare services. There is low government contribution and high private share in healthcare. This leads to a huge gap in healthcare funding which is increasing the individual out of pocket expenditure with no social coverage from the government. (The World Bank) Availability of essential drugs in public healthcare facilities is another challenge. Thus the state needs stringent implementation measures to address the access and affordability of healthcare.
Maternal mortality and lower coverage of antenatal, natal and postnatal care is another challenge in the state. Though this has come down in the state largely but still needs some improvement. As mentioned above strengthening rural health infrastructure can help in achieving the coverage of maternal and child healthcare services. Maternal mortality in the state is also emerging from inadequate awareness of maternal complications being the main. Unavailability of transportation and skilled workers is another preventable measure of maternal mortality. Hence the reach of institutional deliveries and PMMVY is low. Economic deprivation among a large population in the state also influences the dietary practices and women’s decisions around her reproductive health and decision making. Many social and cultural factors further deprive the women from adequate nutrition intake along with household burden of work and care giving roles. In the state deliveries continue to take place at home attributing to resistance by family members, lack of knowledge and accessibility. Sahiya workers play a crucial role in shaping such decisions. With their support and awareness creation, there is an increase in institutional deliveries and antenatal check-ups hence the gap of availability and capacity building of them needs to be addressed for their effective functioning.
In conclusion, it is evident from the studies that Jharkhand has a high percentage of vulnerable population with economic and social deprivation. Regional differentials show the north eastern and southern region are far behind in socio-economic development than other parts and also in utilization of maternal and child health care services. Mothers education, birth order, wealth index are the most important determinants in Jharkhand. 36
Hence, policies and programs must focus on backward regions and poor socio-economic groups in order to abridge inequalities prevailing among them.
- RECOMMENDATIONS
There has been a momentum in improved maternal and child health in the state in the last few years but still there is need of strengthening it further. Through this paper we put light on recommendations for both government and CSOs to work in alignment. Hence, following are some recommendations which could be incorporated.- State can incorporate in providing a hot cooked meal food for pregnant and lactating mothers in the anganwadi which could further improve the diet diversity and nutrition intake of the mothers. Similar models have been adopted and shown positive results in Karnataka, Telangana and Andhra Pradesh.37
- Special attention should be to the Tribal Districts as they report high levels of wasting, underweight and stunting.38
- Monitoring of implementation of Pradhan Mantri Matru Vandana Yojana PMMVY should be strengthened. Adoption of good practices can be considered like Odisha’s state run maternity scheme covers 2 children, and this practice reported improvement in awareness levels, application rates, and actual benefits. 39
- The upholding of reproductive and sexual and health services are essential to supporting human rights. Therefore, policies and programs must address comprehensive reproductive rights beyond maternal health and contraception; they must encompass a gamut of imperatives like WASH practices, education, freedom from violence; accessible and quality care for abortion.
- Adolescent centric health policy can boost the ongoing planning around improved maternal and child health. Nutrition support to adolescent girls, knowledge around menstruation health and hygiene, violence and mental health has a direct impact on overall health. Jharkhand Initiative for Adolescent Health (JIAH) is one such trial in rural Jharkhand which has improved their knowledge and action on education, nutrition, violence and health.
- Much has been done around the capacity building of Sahiyas. Jharkhand should prioritise building strategies to strengthen primary health care services throughcapacity building of AWWs and other ICDS functionaries.
- There is a need to strengthen the existing Public Health facilities to meet standards set by the Indian Public Health Standard (IPHS). Speedily steps are required to address the gap of skilled human resources along with availability of health infrastructure, service facilities and medical supplies.
- Considering the ongoing pandemic, there is a need for strategies to promote psychosocial wellbeing by meeting urgent mental health needs as well as necessary mental health care provisioning in the long term as part of comprehensive healthcare.
- COVID 19 response & reallocation of health services should not undermine the access to essential comprehensive abortion care.
Following are the recommendations for the CSOs to support in providing better healthcare:
- Review system of PMMVY could be scaled up to ensure timely coverage of early registration of pregnancy, antenatal and postnatal checkups. CSO and the Health departments together can impact the service utilization through community training and awareness impacting their health seeking behaviour. Creation of a forum within village/SHG can lead to strong efforts towards improving maternal health and can serve as a support to Sahiya.
- CSOs can help in systematising things for better monitoring and implementation of services.
- Interventions around improving WASH practices and functioning of water and sanitation committees can improve health outcomes.
- Strategies to increase the coverage of Wellness centres and their functioning can address the socio cultural factors influencing health through awareness creation. Collaborations with CSOs can be effective for Capacity building of health workers.
- Actions in rural health cannot be initiated without promoting an interdisciplinary perspective and a culture of complexity and reflectivity. We need to consider local populations in transition and not in a fixed homogenous situation by taking into account local disease classification and local pragmatic solutions through a dialogue between bio-medicine and therapeutic pluralism.
- Recognise gender based violence (GBV) as a public health issue and draft clear guidelines for an action plan. There is an urgent need to set up help lines and help desks for women in their close proximity. This should be done through a consultative process with women’s groups and public health organisations working on gender based violence.
Under NHM, another initiative of the Government is the Mobile Medical Unit per district as an effort to provide health care at the doorstep. In Jharkhand, through Public Private Partnership Medical Units (MMUs) has been started from the year 2008 in all 24 districts. Despite the poor condition of the road, and the unwillingness of doctors to go to far-off areas, it has reached many and improved their access. 13
● Rashtriya Bal Swasthya Karyakram:
This aims to provide comprehensive child health care to prevent, manage and control diseases, deficiencies, and disability and development delays. These delays may lead to permanent disabilities if timely intervention is not done. Thus, program focuses on their early detection and management along with addressing other factors to prevent these. This aims to provide comprehensive child health care to prevent, manage and control diseases, deficiencies, and disability and development delays. These delays may lead to permanent disabilities if timely intervention is not done. Thus, program focuses on their early detection and management along with addressing other factors to prevent these.
● Sexual and Reproductive Health
Sexual health and well-being is recognised as an indivisible aspect of human rights that includes physical, psychological, social and epidemiological aspects relating to sexuality.
India was the first country in the world to have launched a National Program for Family Planning in 1952 and has undergone transformation in terms of policy and actual program implementation. ASHA spread awareness and delivered contraceptives to people at village level and also counsel the newlywed about birth spacing. Pregnancy testing kits are also made available by them. 14